Health Center Partners and Our Family of Companies' Impact Reports
2023
February 2023 | Health Services Reports
February 2023 | State & County Economic Value & Impact Reports
February 2023 | District-Level Economic Value & Impact Reports
2022
February 2022 | Economic Value & Impact Reports
2021
Infographic: Celebrating Excellence in Health Care
February 2021 | Economic Value & Impact Reports
2020
February 2020 | Economic Value & Impact Reports
2019
June 2019
CA American Indian/Alaska Native Maternal & Infant Health Status Report
May 2019
HCP Member Profile
February 2019
Value and Impact Report for Health Center Partners' Members
In 2017 our 17 members in San Diego, Riverside and Imperial counties:
- Had a Total Economic Impact of $1.712 billion
- Provided 11,412 jobs
- Served 806,158 patients (unduplicated)
- Provided 3.2 million patient visits (unduplicated)
County Level Reports
Imperial County
Riverside County
San Diego County
2018
March 2018
California Health Care Foundation with The MacColl Center for Health Care Innovation at Kaiser Permanente Washington Health Research Institute and JSI Research & Training Institute, Inc.
Partnering to Succeed: How Small Health Centers Can Improve Care and Thrive Under Value-Based Payment
“We now have data that indicate networked health centers outperform non-networked health centers clinically, including UDS data that indicates our HCCN outperforms others across the country in 10 of 13 clinical measures, and HEDIS data that indicates our CIN is posting the highest minimum performance level scores Molina Healthcare has ever posted in California, by any provider group. What that says to me is that the time has come for FQHCs to work together in networks, locally and regionally, to ensure the delivery and continuity of high- quality health care and the highest possible outcomes, at reduced cost, for the patients entrusted to their care. How one does that, through an IPA or a CIN or other vehicle, will have its own pros and cons depending upon the business model and the business goals of the organization.” - Henry N. Tuttle, President and CEO, HCP

March 2018
Advancement Project California, USC PERE, PICO California and California CALLS
Health Care Access: Securing the Counties' Health Care Safety Net for All Residents
The Advancement Project California, USC PERE, PICO California and California CALLS new report analyzes health care access trends in Los Angeles County, Riverside County, and Merced County. The report finds, despite considerable progress made in health coverage, access, and outcomes during the early years of the Affordable Care Act (ACA) implementation, people of color in California continue to face disproportionate obstacles to accessing quality health care. Case studies in Los Angeles County, Riverside County and Merced County that examine post-ACA changes reveal lessons learned in each region and opportunities to reduce disparities and increase access
“Community health organizations are filling a vital need in Riverside County by providing affordable, high quality, and culturally competent care to many of our most vulnerable residents,” said Vernita Todd, senior vice-president of external affairs of Health Care Partners of Southern California. “Adequate investments in community health clinics can help close gaps in access in a County that is as large and diverse as Riverside.”
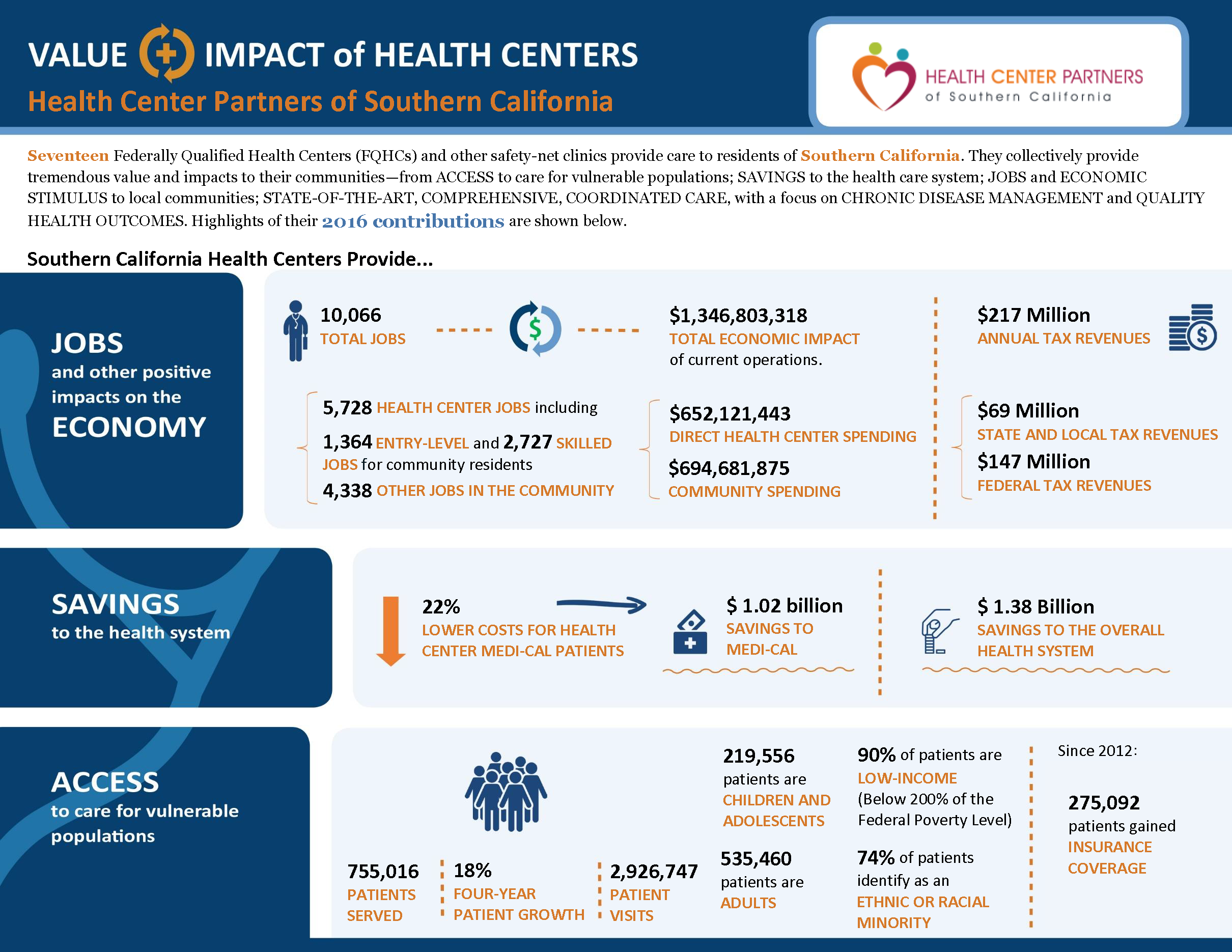
February 2018
Capital Link
Value and Impact Report for Health Center Partners' Members
- Had a Total Economic Impact of $1.34 billion
- Provided 10,066 jobs
- Served 755,016 patients (unduplicated)
- Provided 2.9 million patient visits (unduplicated)

March 2018
The Joint Commission Journal on Quality and Patient Safety
Margaret Meador, MPH, C-PHI; Jerome A. Osheroff, MD; Benjamin Reisler, MPH
Improving Identification and Diagnosis of Hypertensive Patients Hiding in Plain Sight (HIPS) in Health Centers
The project used a quality improvement approach wherein information flows and actions related to blood pressure measurement were modified to include algorithm criteria to identify patients who might have undiagnosed hypertension. Identified patients were recalled for evaluation and hypertension diagnosis, if appropriate. Ten health centers in Arkansas, California, Kentucky, and Missouri were selected to participate in the project on the basis of high hypertension prevalence (compared to national average), demographic and geographic diversity, mature information systems infrastructure, and executive support. The project targeted patients from 18 to 85 years of age.
2017
March 2017 | Capital Link
Value and Impact Report of Health Center Partners' Members
Seventeen Federally Qualified Health Centers and other safety-net clinics provide care to residents of Southern California. They collectively provide tremendous value and impacts to their communities—from JOBS and ECONOMIC STIMULUS to local communities; SAVINGS to the health care system; ACCESS to care for vulnerable populations; STATE-OF-THE-ART, COMPREHENSIVE, COORDINATED CARE, with a focus on CHRONIC DISEASE MANAGEMENT and QUALITY HEALTH OUTCOMES.
2016
December 2016 | National Association of Community Health Centers
Partnership Shows Quick Hypertension Control Returns
October 2016 | National Association of Community Health Centers
Community Health Center Workforce and Staffing Needs
July 2016 | California HealthCare Foundation Report
San Diego: Major Providers Pursue Countywide Networks and New Patient Care Models
May 2016 | Prepared by Rafael A. Gomez and Bobbie Wunsch of Pacific Health Consulting Group
Ready, Set, Enroll : Community Health Center Strategies to Enroll Undocumented Children into Medi-Cal under the Senate Bill 75 Medi-Cal for All Children Expansion
Funding for this report provided by Blue Shield of California Foundation
May 2016 |National Association of Community Health Centers
Women’s Reproductive Health: FQHC Requirements
January 2016 | WORKFORCE REPORTS via CPCA and NACHC
HORIZON 2030: Meeting California’s Primary Care Workforce Needs (CPCA)
STAFFING THE SAFETY NET:Building the Primary Care Workforce at America’s Health Centers (NACHC)